Who decides whether someone’s treatment for a mental health or substance use disorder is ‘medically necessary’? Or how long treatment should continue, or in what setting?
I think most Americans would answer: “The insurance company, naturally.” And grimace as they do, because they (or someone they know or have read about) went through the arduous process of challenging a company’s decision to refuse payment for care.
But that situation got a lot better after a 2019 decision by the district court in San Francisco. It effectively returned control over such matters to the clinician, working with the patient and family to achieve the best possible outcome. Observing a set of principles known as “The Eight Generally Accepted Standards of Care.”
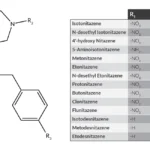
If you’re not familiar with them, here they are:
- Effective treatment requires treatment of the patient’s underlying condition, not just alleviation of the patient’s current symptoms.
- Effective treatment requires treatment of comorbidities in a coordinated manner that considers their interactions when determining the appropriate level of care.
- Patients should receive treatment at the least intensive and restrictive level of care that is safe and just as effective as a higher level of care.
- When there is ambiguity as to the appropriate level of care, the clinician should err on the side of caution by placing the patient in the higher level of care.
- Effective treatment includes services needed to maintain proper functioning or prevent deterioration.
- The appropriate duration of treatment is based on the patient’s individual needs, not on a specific limit on the duration of care.
- The unique needs of children and adolescents must be taken into account.
- The determination of the appropriate level of care should be made on a multidimensional assessment that takes into account a variety of information about the patient.
“That’s definitely patient-friendly,” a colleague of mine remarked. And family-friendly, too. Hard to imagine many clinicians who’d disagree. From their perspective, it’s just sound practice in terms of preserving safety and delivering quality treatment.
On the other side of the equation, many in the insurance world were downright unimpressed. Who’s going to pay for all that? they wanted to know. Not us.
In March of this year, the lower court’s decision was reversed on appeal. So much for the Eight Standards, I guess. The timing couldn’t be much worse, given the pandemic-related explosion in mental health problems. And with fentanyl replacing heroin as the opioid of choice on the street.
Tom Insel, a psychiatrist and former Director of the National Institute of Mental Health, has written about this issue in Psychiatric Times. Here’s the link, which I hope you’ll take advantage of:
Federal Court Gives Green Light to Deny Coverage
We’ll be returning to this subject in future posts, as I expect it will continue to be a prominent topic in the coming months.