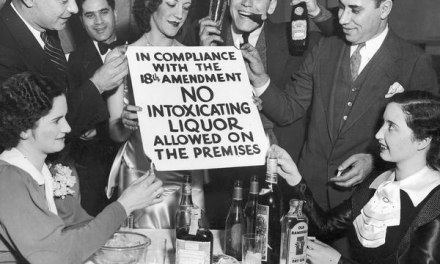
Here’s a fascinating article on the role of current neuroscience research in understanding pain– of special interest to the addictions field since it was the treatment of pain with opioids that helped create our current epidemic. We shouldn’t forget that strong efforts to make opioids more available haven’t stopped. There are still patients in extreme need, unable to function without them, as well as pharmaceutical firms anxious to protect their revenues.
As you know, the problem of pain is now divided into two broad categories. There’s acute pain, which ordinarily follows some type of injury or illness. It’s generally sharp and severe and lasts a few weeks or months, no longer. Then there’s chronic pain, that persists beyond initial months and may lack any clearly defined source. It can be even more disabling since it refuses to go away.
Acute pain is considered a response to injury or illness, while chronic pain is viewed as a disease process in and of itself — one that requires treatment beyond an initial injury.
Several psychological factors have been shown to exert influence over our perception of pain, and therefore, our ability to cope with it. Depression, for instance, will affect the way we perceive and rate painful stimuli. So can anxiety, anticipation, or even distraction.
Researchers have used functional imagine (fMRI) to map the brain activity during the experience of pain. The goal is to eventually develop an objective scale by which pain can be measured not by self-report, but by neuroimaging. This would replace our current reliance on subjective self-ratings– the one to ten scale, for example, or the “smiley-face” test.
Because we lacked objective measures, we’ve had no end of problems both in law and healthcare. Doctors are forced to prescribe based on patient complaint, without objective confirmation. Likewise, lawsuits that include requests for compensatory damages for pain have to be negotiated on a case-by-case basis. As the article points out, if we had an agreed-on system of measurement for pain, those cases could be settled without litigation.
As for chronic pain, medicine has likely been overreliant on long term opioid therapy, often at high doses. Turns out that can engender a condition known as hyperalgesia, or an abnormal sensitivity to pain. That’s not detectable on subjective ratings like the smiley-face test. But the implication that in using opioids in this fashion, we may inadvertently have worsened someone’s pain.
To me, it’s like treating hypertension without access to a blood pressure cuff. How much confidence can we have in what we do?
Let’s hope research helps us out.