About those supplements that seem to take up so much shelf space in our grocery and natural food stores – how much value can they actually bring, to someone in early recovery? In this instance, for common complaints of depression and/or anxiety?
Science has an answer: some value, perhaps, limited to some cases. But science cautions against expecting too much from a supplement.
And there are also risks to consider, if you’re taking prescribed medications as well as the supplements.
Still, it isn’t hard to understand why supplements are so popular. First, they’re much cheaper than most prescribed meds. Second, you don’t need a doctor’s permission. And look, it says right there are on the package, it’s been ‘proven effective’. They couldn’t say that unless they had proof, could they?
Yes, they could. And often, they do.
I noticed that the questionnaire the nurse asked me to complete (prior to being admitted to the presence of an actual physician) had been updated to include a question about any nonprescribed vitamins, supplements, or other so-called ‘natural’ remedies I might be taking. And if so, then what were they, and how much did I take, and how often?
The nurse went on to explain that many so-called ‘supplements’ had been found to interact poorly with medications that physicians often prescribed. This applied not only to heart, lung, immune, and related problems, but for mood and anxiety symptoms as well. As the latter are quite common among folks in early recovery from SUDs, I figured it was worth looking into.
Here’s something on the subject that turned up in a recent issue of The New York Times.
Can Supplements Really Help With Depression and Anxiety?
The newspaper went to the trouble of reviewing a number of the most popular health-food supplements that claimed to provide symptom relief. Among their conclusions:
St John’s Wort: This may be the most widely publicized of natural remedies for depression. The NYT article reports that some research evidence exists for its effectiveness with depressed mood (the mild to moderate sort), but the findings have yet to be confirmed by later, better designed studies.
To date, the evidence in favor of St. John’s Wort is not strong. If it were to be submitted to the FDA for approval, it would likely fail. That’s one reason to keep St. John’s Wort in the Wellness section, instead of behind the Pharmacy counter.
Then there’s the issue of potential interaction between the Wort and mainstream drugs such digoxin (cardiac disease, irregular heartbeat, etc.), warfarin (blood clotting), and theophylline (breathing difficulties), among others. There, the recommendation is to be sure to consult with your physician before adding it to your routine.
Omega 3 Fatty Acids: Also very popular in the mass market, they too follow the same pattern, research-wise: limited positive findings early on, enough to inspire initial hope, but nothing that held up well under further scrutiny from research.
L-methyfolate: Ironically, this folic acid supplement, which is also found in certain foods, appears to work better when used along with a regimen of prescribed antidepressants. Not sure why that would be, but it’s clear that with respect to symptom relief, the prescribed meds do most of the heavy lifting.
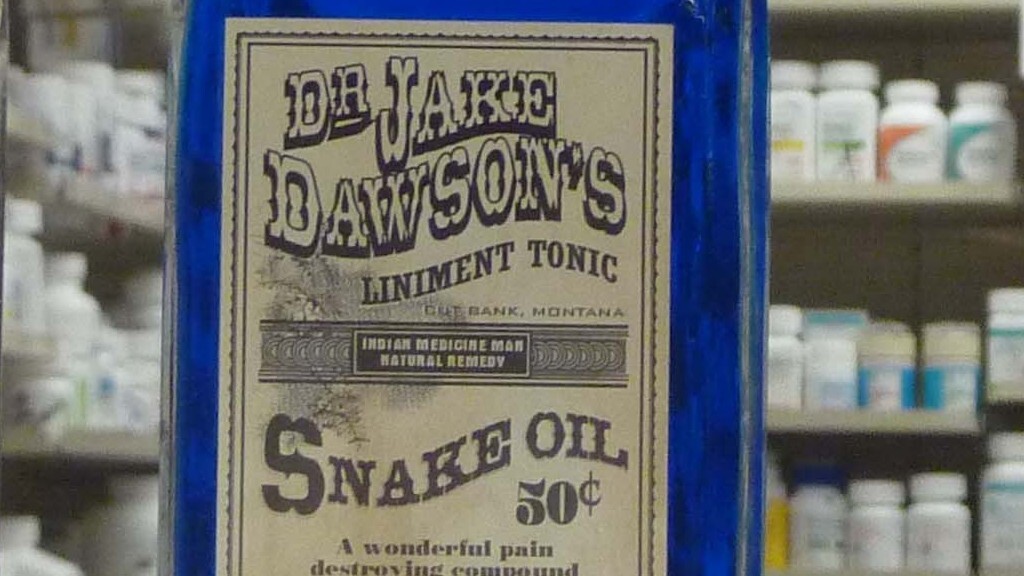
How do most of us initially learn about these and other preparations? From friends and associates, obviously, but increasingly from television. TV has never been the most reliable source for medical advice. The Dr Oz show is just one highly publicized example, among many. He himself is a qualified physician, but the advice he dispenses so freely is subject to heavy criticism within the healthcare professions themselves. “Little more than snake oil,” sneered one commentator.
It’s enormously profitable, however, for the sellers. Take Alex Jones, whose legal problems have led to disclosures of the revenue he has generated from near-continuous promotion of supplements on his program. The numbers being bandied about are astounding.
When it comes to anxiety, the Times article mentions three preparations in particular: valerian root, lavender, and kava. The third has become fashionable in the past decade, and is now even available at dedicated ‘bars’. WebMD says this about kava.
Again, it’s easy to see why any prospective user should check in with the physician before committing to it, especially if they’re on any prescribed medicines that could potentially conflict.
About the loose rules around supplement use: The NYT article quotes an industry rep who explains that, so long as no claim is made for the product as a treatment or cure for any specific disease or condition, then the makers and sellers “…can say anything they want to” about its supposed benefits. I imagine that’s why supplements are often advertised as curing several different ailments rather than one. It’s a truly big loophole that supplement companies are more than happy to drive their delivery trucks through.
As for what might actually be of genuine help to someone in recovery yet dealing with depression or anxiety, the article recommends exploring TMS, which has been subject to FDA approval. You’ll need a professional for that, however. Here’s an overview from the Mayo Clinic.
They also suggest getting more exercise, pointing out that exercise, at least, is still ‘free’.
Obviously they never had to join a gym.