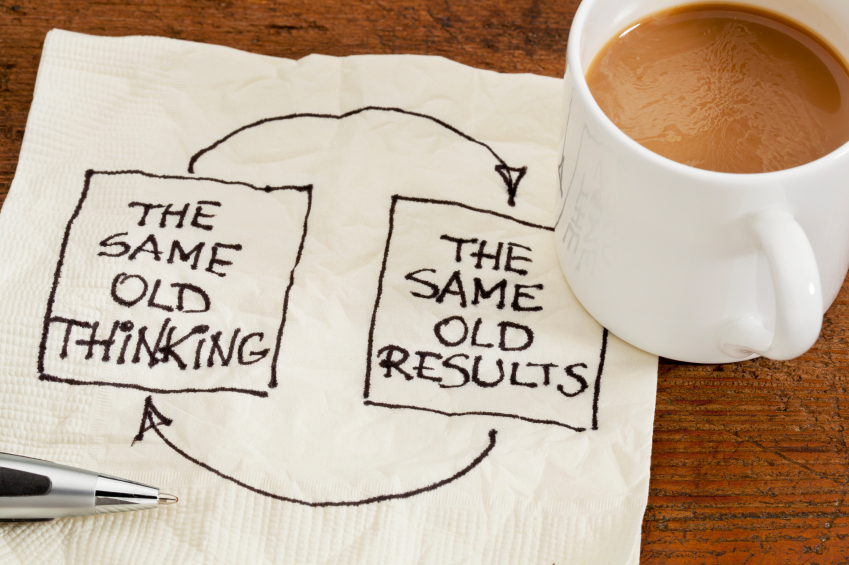
I’m following up on an earlier post on the subject of the so-called ‘Hardcore’ recidivist in addiction treatment – the one with numerous prior treatments, all followed by a return to substance use. We’re left wondering what to do.
Part of the solution can include understanding and addressing, in the context of therapy, secondary gain attached to the behavior. It’s something the relapser may not be aware of. In fact, in my experience that’s usually the case.
I should clarify: By secondary gain, I’m referring to a psychological or emotional advantage or benefit that occurs from an illness or behavioral disorder.
It’s different from a secondary agenda, where the perceived advantage is mainly a practical one. An example of the latter: the Medicaid administration in one state decided to severely limit access to inpatient psychiatric units unless the patient was assessed as actively suicidal. The intent was obviously to reduce inpatient hospitalizations and save money. Word spread quickly on the street and soon ER waiting rooms were filled with folks who insisted that unless admitted to the hospital, they’d no doubt kill themselves. Some meant it, but once on the inpatient unit, others confessed they’d simply been looking for a way onto the psych unit.
“Why don’t you just head on over to the Ninth Street Shelter?” I asked one fellow. “Shelter don’t give you no meds,” he pointed out, clueing me in.
Anyway, secondary gain is more complex. I’ve encountered it with other repetitive behavior patterns. Certain types of self-harm, such as cutting or burning, for instance. Seen perhaps most commonly but not exclusively among adolescents and young adults.
For a long time, rehabs responded by rushing the youth to the ER for prompt medical attention. As the years passed, however, therapists began to suspect that was actually reinforcing the behavior, which in itself wasn’t reliable evidence of true suicidality. They changed the response, and there are now fewer ER visits.
With ‘hardcore’ addiction relapse, it can be important to explore two factors. First, what benefits, emotionally speaking, might be gained from such persistent ‘failure’? Is it failure at all, or a weird kind of success at demonstrating something important to others? Proving some point to current family, for instance, or in the context of family of origin?
Second, what benefits might be lost if the pattern of relapse were to stop, once and for all? What would that mean in terms of the future?
Yeah, I know, it’s a bit therapy-ey for my taste, too. But sometimes yields an insight that can be helpful in changing behavior.
More on this later. Don’t expect the client to have the answers ready and waiting. It may take some time.