A recent study led the authors to conclude that medications that might help alcoholics were greatly underutilized by treatment professionals. Based on long experience, I’m not so sure.
We’ve talked before about the difference between efficacy and effectiveness. Outcomes obtained in a research environment may not carry over very well into actual practice. That’s often the case when the target patient has a history of difficulty taking medications as prescribed.
There are a number of alcoholics who fall into that category.
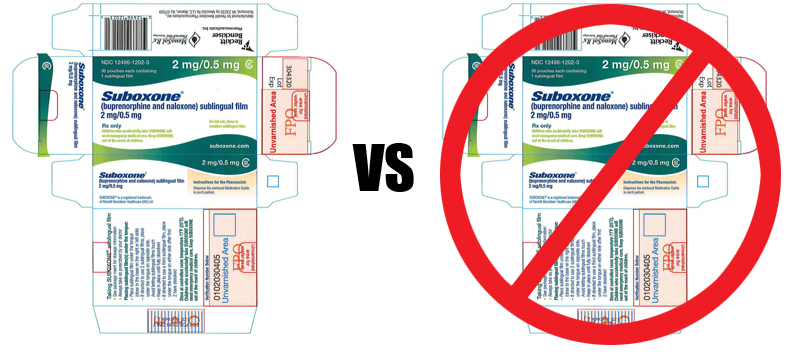
We worry about alcoholics taking too much medication, but surprisingly, they may also be taking too little. One study found that patients supposedly on Antabuse were taking it so infrequently that their blood levels were insufficient to produce the desire response. In other words, useless. The same issue has come up with oral naltrexone. “I’ll take some if I feel like drinking,” the alcoholic may think to himself, but after a couple drinks, the resolution vanishes.
Studies may evaluate medications for alcoholics in terms of fewer drinks per occasion or fewer drinking occasions per week or month. In other words, the alcoholic is still drinking, just drinking less. Instead of being used to facilitate sobriety, the med is being used to facilitate continued drinking. So the alcoholic is still at risk for adverse consequences that may stem from mixing alcohol with the medication.
Also, many studies aren’t that long-term. Three months is common. An alcoholic can self-regulate consumption for periods given the support from a research project, but when that support ends, a return to previous behavior is likely. That behavior may not be worse than before the study, but it may not be better.
Healthcare practitioners prescribe medications to alcoholics in expectation of improvement. That expectation may be based on something read in a journal, or on experience with another patient. But in real-life, there may not be the opportunity to follow closely enough to see if hopes are realized.
I do think many addiction professionals are cynical about the use of medications, outside of detox or the treatment of a concurrent mental health disorder. They do get accused of being Puritans, but what they may really be is experienced.