For Opioid Use Disorders (OUD), at least. The FDA has actually approved a commercial product to identify OUD risk in patients who have no known history of opioid misuse.
Be great to have, but I can’t help wondering how well that would work in practice.
By way of background, there are a number of new products on the market for physicians to use to predict patient’s response to various drugs. An example: The wildly popular GLP-1 medications — you know them better as Ozempic (for diabetes) and Wegovy (for weight loss).
The idea is that the gene test would aid doctors in deciding who might be a good candidate for either. We already know that some people respond better to GLP-1 than others do, but we can’t predict in advance who they may be. If this test works as hoped, it would presumably become part of the routine exam when the drugs are prescribed.
Useful, no? At the very least, it’d lower the risk of a disappointed user when the “miracle” med fails to produce the desired outcome.
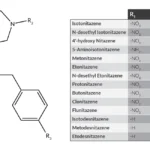
Of particular interest to us, there’s also a genetic test, recently approved by the FDA, that claims to predict a patient’s risk of developing an Opioid Use Disorder. The idea is that physicians would use it to determine the potential for misuse or abuse of the opioid before they prescribe it — for instance, after surgery.
The FDA-approved test is named AdvertD, and involves a simple swab of the patient’s cheek. Sounds terrific, but it seems to have triggered a wave of protest from a prestigious group of physicians. Including Andrew Kolodny, whose work I have respected for years.
Quoting Dr. Kolodny: the test offers users “… the appearance (italics mine) of predicting genetic risk, without being a true measure of genetic risk.” The experts go on to assert that “Patients who test negative, and their clinicians, may have a false sense of security about use of opioids…”
We don’t want that, especially in view of the origins of the prescription drug epidemic — founded on a false sense of safety related to the risk of addiction from long-term opioid use.
At the time, we were told that was safe.
How’s the saying go? “Fool me once, shame on you. Fool me twice, shame on me.”
The objection also works in reverse. A physician might be reluctant to prescribe enough opioid medication to control a patient’s pain, all because of a misleading result from a genetic test.
Sounds as if the experts who sent the letter lack full confidence in the test itself. What did the study show? That the test correctly identified patients with OUD in about 83% of cases. In the other 18%, it yielded a false negative.
There was a false positive in around 21% of the cases.
Both the false positives and the false negatives seem a bit high to me, given what’s at stake for the patient.











Having just watched Dopesick about PerduePharma’s aggressive drug pushing of their OxyContin to the tune of hundreds of thousands of fatal overdoses, it sounds like this would be their next drug for Season 2.