I’m a counselor at a residential recovery program in a small town. There aren’t many halfway or transitional options for us to refer clients to when they’re discharged, so our main aftercare focus is on finding good recovery support. AA and NA are available here or in nearby communities, with several solid meetings. Lately I’ve been hearing some resistance among my colleagues, to referring clients to these groups. Is there something I should know?”
To revisit some of the common problems cited by professionals who won’t refer clients to 12 Step groups:
The client reports having had a bad experience, recently or in the past. This is very common, and newcomers are particularly susceptible to any sense that they’re not welcome. Many clients interpret this as a sign to give up on the fellowship, when in reality, it’s a signal to explore for more compatible meetings. In one community, the main Sunday night AA meeting developed a rep for attracting those looking for love rather than sobriety. The treatment program removed it from the recommended list for its clients, and started its own women’s meeting, using a strong core of peer support staff and recovering volunteers.
This is also an opportunity to work on an all-important issue in early recovery: personal boundaries. “I learned early in my career how to set limits on people,” one psychiatrist related. “In medical school. I was one of just a few women. You learn to draw lines and hold them.”
The client received some bad advice at the 12 Step meeting, usually about treatment, including medication. There was a longstanding prejudice within 12 Step culture against the use of drugs in recovery, and like most things in the fellowships, it was based on experience. But that prejudice has eroded over the past few decades, mostly due to education by treatment programs. Patients are now taught about the role of medication and how to handle questions from others. There’s still a popular bias against people on opioid maintenance—some NA members consider them ‘not actually in recovery,’ but now meetings for OMT clients are fairly common, and where they aren’t, clients have developed workarounds. One man revealed to his sponsor that he’d secretly been on buprenorphine for the entire three years he was attending meetings, and was just now beginning a taper. His sponsor’s reaction: Why didn’t you tell me? Plus congratulations on his success so far.
The religion issue. This works both ways. We all know people for whom any mention of God is one mention too many. And there are religion-based fellowships that are quite opposed to the 12 Step brand of nondenominational philosophy. Folks who have really strong prejudices on either side aren’t likely to succeed in AA or NA, if only because they won’t attend. Nonetheless, it’s good for every program to present options. We encourage treatment centers to offer homes to meetings of local support groups, regardless of philosophy.
Our point is that like any other barrier to doing something that could ultimately benefit your recovery, the above objections can often be overcome, through counseling. Provided the therapist is willing to make the effort.






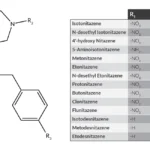







Great advice overall but the reference to opioid-replacement as “…not being in recovery..” is misleading. There is no question that those using srug-replacement therapy are recovering, at issue is whether or not they meet the NA/AA definition of abstinence, meaning being ‘clean/sober’; which they do not. There are other mutual aid groups and ’12 Step’ fellowships (like Methadone Anonymous) where these individuals may find greater affinity. NA/AA are not for everyone but they are the perfect solution for some; let’s not threaten their recovery by trying to make NA/AA a ‘one size fits all solution’.