I’m using ‘tail’ in the sense of an increased risk for a range of health problems in the future — as evidenced by a recent study described in The Lancet.
Researchers examined the relationship between past hospitalizations for a Substance Use Disorder (SUD) and future occurrence of common medical problems and conditions. Twenty-eight of them, in total.
Their sample was very large, drawn from the population of the Czech Republic. Their conclusion: If someone was sick enough at some point to have been hospitalized for treatment of an SUD, they are statistically more likely to suffer from other medical problems later in life.
No, it’s not exactly good news, but it shouldn’t come as a total surprise, given the damage associated with serious substance abuse. When it comes to SUDs, hospitalization is seen as evidence of a higher level of acuity — the need for 24 hour medical supervision and monitoring suggests an advanced case.
Here’s a link to the summary, if you’re interested:
Their advice: “Clinicians should take note of such clinical histories and ensure that patients with previous hospital admission for substance use disorders are given high-quality integrated treatment.”
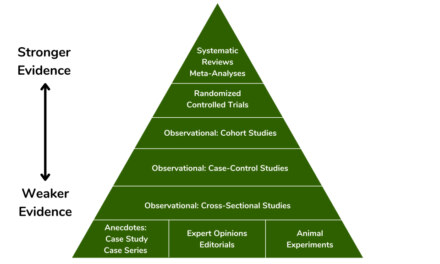
Gotcha. So how might this knowledge- assuming it is confirmed by other research — affect our approach to treatment? Perhaps it could present addiction treatment professionals with an opportunity to increase patient awareness and provide early education and intervention in at least a few important areas.
That would seem to be an advantage not only to patient, but to the family and the community as a whole. That’s particularly true for disadvantaged populations where rates of disease may be higher, and access to good healthcare perhaps less available.
For instance, the researchers advise ‘high quality integrated treatment’, suggesting links between addiction programs and primary healthcare providers, permitting true coordination of care. There’ve been efforts to achieve that goal in the past. I believe results have been mixed.
I’m thinking of one state where addiction programs were required to initiate contact with a newly admitted patient’s primary care provider (PCP) to establish lines of communication between the two. In practice, that involved a letter that went to the PCP explaining that the patient had been admitted for SUD treatment.
The letter asked for a response from the PCP — this was a Medicaid population, so the PCP was usually at a clinic — but as I recall, seldom got one.
One program dispatched a member of its community outreach staff to visit the largest local family medicine clinic, in hopes of finding out where and why the process was breaking down. She met with staff members over lunch, reporting back that the clinic staff seemed to feel that dealing with drug and alcohol problems was somehow not part of their role.”The medical consequences, sure,” she explained. “But not addiction. They felt that was our job, not theirs. Their focus had to be on the physical stuff.”
Ahah. I wondered what they did with the letters we sent. Filed them somewhere? Tossed them in the trash?
I’ve noticed that this kind of thing occurs when a regulation is made to ensure that something is done but the process to complete it hasn’t yet been developed. It leads nowhere, like that famous bridge in Alaska.
That sort of fragmentation Can be found all through healthcare, despite the dogged efforts of some very smart people to fix it. “Communication,” one of my own treating physicians sighed, when he was told test results he was waiting for had simply never been sent. “It’s just not our strength.”