By this time, we have access to some genuinely useful research into cannabis as a health hazard– not just for users, but those around them. Here’s recent example:
Helpful research is important when we’re on the verge of an era of legal cannabis use. As of this writing, 11 states have made recreational use legal, with more on the way. A total of 35 have active medical marijuana programs. The rest continue to observe the Federal law, which still treats cannabis as a Schedule 1 controlled substance.
Years ago I worked with man in his early 30’s, a daily pot user since his late teens. He’d be a ‘chronic heavy user’ in today’s jargon. Once he and his wife began to have kids, she became increasingly uneasy with the practice. They struck the usual deal: he agreed to confine his pot use to places outside the home, and to never smoke in front of the kids. As the children grew, however, things changed. His wife complained about the strong odor and how he often looked and acted stoned in front of the children. After months and months of ‘discussion’, he finally threw up his hands and agreed to give up pot altogether.
This happens quite often. Family and job responsibilities are a common motivation. For instance, he taught junior high. Drug use was prohibited by school policy, so there was always the risk that it could become a career issue. It hadn’t yet, but even he could appreciate the danger.
Anyway, his plan was to head for a remote cabin in the mountains, spend a week by himself in the absence of marijuana. A form of cold turkey detox, he called it. He returned home feeling better, proud of his success, and ready for a new start.
At some point, however, his family — children and wife — began to hint that maybe he wasn’t so pleasant to be around. Irritable, impatient, quick to snap at people — definitely not his former self. There was a suggestion made that perhaps he could reintroduce cannabis, cautiously. He did. I don’t know how it all turned out.
Now, given research on the second-hand effects, I’m realizing that marijuana, legal or not, can be a problem for people around the user. For a long time they felt they had to put up with it, the way folks used to feel about cigarette or cigar smoking. Research into secondary smoke played a big, big role in changing that.
I’ve said before that it’s likely that clients in treatment for alcohol, cocaine, opioids etc., will want to continue using cannabis. “I never had a problem with grass,” they’ll argue. “I’m giving up heroin (or alcohol, cocaine, et al), but why should I give up weed too?”
Cannabis, particularly in its more potent forms, does alter how people think and feel. Not that the user is always aware of that. I listened to staff at a large methadone clinic complain about it. “They say they didn’t smoke the day of the session,” was the refrain. “But they’re stoned. You can’t miss it. Or they don’t show up at all. Seems like sooner or later, it becomes an obstacle in treatment.” We can’t forget that treatment clients are generally later stage, with longer histories, and are more severely dependent on substance use. Their tendency is towards lapse and relapse. It’s stable recovery that represents the challenge.
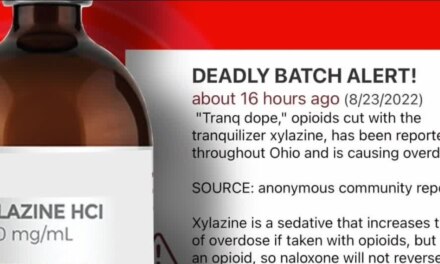
So how do treatment programs, especially outpatient, deal with it? Some make it an issue, while others ignore it. “It’s not good,” one clinical director admitted, “but at least they’re not using heroin or fentanyl.” For now, at least. So far as we know.
It’s plain difficult for many patients to give up one intoxicating drug while continuing to use others.
Harm reduction value aside, I think we can do better.