We hear it a lot in the counseling field — the key to success is retaining the client in treatment.
A very intuitive notion. After all, unless the client is participating, how can he possibly benefit?
And research does suggest that staying in counseling for at least 90 days is important in terms of getting the optimal results.
No argument there. That line of reasoning has generated a rash of enthusiastic efforts to improve retention rates. For some programs, it’s become the ultimate success measure.
But sometimes the program forgets to answer the really important question: is the client actually making progress? The measurable sort, in relation to goals and objectives.
Treatment is supposed to produce positive change. Otherwise there’s no real point to it. We have no cure, so even in remission, the client is still an addict. The challenge is to sustain the remission, going forward.
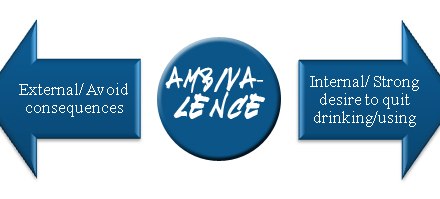
That goal requires substantial behavior change. I’m using behavior in the broad sense – not just actions, but thoughts and feelings. Success requires change with respect to all three.
That is, if the addict is to make the difficult transition from a life devoted to drug-taking to one devoted to recovery. It ain’t easy. Few things we ever do will prove anywhere near as challenging.
So treatment has a responsibility to actively promote change.
I’m a fan of client-centered therapy, but we shouldn’t go overboard. The client should direct the course of treatment, but not in any direction he feels like taking it. That’s not how we accomplish important goals. We do that through focus.
Treatment needs to move proactively towards the changes needed for sustained recovery. If it isn’t, then it may be treatment for an addict, but it’s not addiction treatment.











I think in outpatient settings having more peer support along with counseling would be more beneficial. The client has to have some willingness and if court ordered if they aren’t making progress then cut the ties. Where I see people struggle the most is after residential and outpatient. It took me a year of my sponsor repeating the same stuff before I gave in, and was willing to completely dive in. People need the most people who have the solution and outpatient only lasts for so long and putting a bunch of people without the solution together for 3 months is not the best path. Team effort both professional and loved experience.
Hi Tim — good idea, maybe I’ll do an article on it. In the interim, we got some good ideas out of TIP 42 on co-occurring disorders, and on TIP 47 on IOP treatment. Both free by download from SAMHSA. Incentive programs like the PAMI stuff are shown to be helpful with retention. But I usually start with looking at the client population — which CODs are most common? How severe the impairment in function? Then I reverse the question. Instead of asking how to increase retention, I ask myself: what barriers do clients encounter when they try to stay in treatment? Assuming you’ve engaged them initially, of course. Are there logistical barriers? Stigma barriers? Motivational barriers? and so forth. Then I address those.
If I had to sum it up, I’m always looking to identify and remove barriers.
I work with people who have cooccurring disorders. I am good with the action stage. I struggle with retention. Any suggestions