I was pleased to hear that the folks at IRETA— the Institute for Research, Education and Training in Addictions– have taken on a project I find of particular interest: The value and viability of providing more intensive treatment services in a methadone maintenance program.
They’ve partnered with Southwest Behavioral Health Management and Foundations Medical Services, LLC (FMS) on a two year project that began about 9 months ago. So far, things appear to be going well. If that holds, I’d hope the final product would be available for replication in other opioid treatment settings.
Currently, the regular opioid treatment program (OTP) schedule includes two and a half hours of counseling every month– one hour with a primary clinician, plus 90 minutes of other activities. The existing program offers considerable flexibility. A client struggling to adapt to medication could attend a special activity.
What hasn’t been readily available is a cohesive group therapy where 10-14 clients could bond with one another around their shared recovery. That’s the basic unit of most drug-free approaches. What would happen if it could be incorporated into the OTP curriculum?
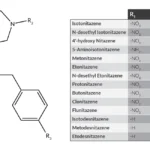
The FMS and IRETA staff decided to pilot a closed, 12 week group experience built around structured Cognitive Behavioral Therapies (CBT). Some of the activities were based on William White’s Recovery Oriented Methadone Maintenance, available here for free.
A single group facilitator is responsible for the entire three months of the program. Client progress is tracked. Participants are asked to rate each session, and their input is then aggregated for review– a real asset for program improvement, but one that’s sometimes overlooked.
The plan is to add other layers of programming as the project matures. A weekly alumni-style group for graduates, for example. And eventually, an IOP component for those who struggle and require added structure to maintain recovery.
The group has only been in operation a few months, but some issues were immediately apparent. The population of addicted people in the group have experienced considerable personal loss, both recent and in the remote past. They’re in need of grief and bereavement counseling. Likewise, there’s a continuing demand for coping skills education: Anger management, stress reduction, conflict resolution, etc.
Oh, and help learning to manage craving. That’s almost universal. Even with medication, participants report periods of drug hunger that, left unaddressed, could quickly sabotage recovery.
As far as outcomes, the program team is focused on the harm reduction measures common to methadone maintenance: Days opioid-free, episodes of other substance use, arrests/criminal activity, high risk behaviors such as IV use. But the therapy itself is recovery-focused.
There’s been much concern about the spread of opioid use to rural environments that rarely if ever saw the problem in earlier decades. This project should provide some insight into treatment of that population. Currently, the group is predominantly white and female.
We may follow up later to see how the experiment is progressing. With so many Americans on maintenance– I’m told more than 350,000, and growing– it’s bound to be worth our attention.










I really enjoyed this. At the program I attend you actually start out in Intensive Out Patient (I.O.P.) that is 3 – 3hr group therapy sessions with a total of 9 hours of group counseling and a half hour of individual counseling per week. After about 6-9 months of total abstinence from drugs and alcohol with clean UDSs in I.O.P. you can move into Out Patient (O.P.) where you do 2 – 2hr group counseling sessions per week and 1hr of individual counseling per month. Than you can move into O.P.2 where you do 1 – 2hr group per week. Eventually you can either slowly detox off of the program or you can move to O.P.3 where you only do an hour of individual per month. This I feel is sufficient therapy and i have seen it work for many but at the same time I have seen the majority of clients stay in I.O.P. where they continue to use other drugs such as Benzodiazapine with methadone to get a Heroin type of intoxication or just continue to use cocaine or anything else with the methadone so they don’t have to go through the opiate withdrawal. It is these clients who are mainly abusing Benzo with their Methadone that give the M.M.T. a bad name and stigma. The thing I see is that for these people there needs to be some kind of time frame that they are allowed to get away with such behavior before they are administratively discharged from the program. I see people still in IOP who have been in the program for 12+ years and still abusing drugs. This i see as a waste of taxpayers money and also pretty much the proof that it is just another way to make money off of a problem that is plaguing our country and our world. There could be so many ways to make M.A.T. so much better but for big Pharma and for the “Man” it wouldn’t benefit their pockets. I am actually working and wanting to be a voice to help change a lot of things within the Recovery world but i am only one voice. I wish I could do more but I definitely want to be a part of the solution and not the problem. Helping others, making a difference, working toward change, and continuing my personal growth is the only thing that keeps me clean. Its about making a change, and giving back. ALL I want to do is help do my part, Give back, and make the world of recovery a place of beauty. Many Blessings,
Kevin A. White
I am glad to see this happening. What breaks my heart is that “norm” for methadone treatment doesn’t seem to include basic substance abuse treatment. Two and one half hours each month?
There are methadone programs that actually require and provide good counseling, based on a thorough assessment and treatment planning process. Our clients start out with 2 1/2 hours of counseling per week, sometimes more, depending on their individual needs. One of those hours is individual counseling. The other is group.
If we are ever to change the stigma around medication assisted treatment, we have to stop treating basic counseling as “optional.” I know, it’s expensive. We don’t rake in big profits. But we keep the lights on and patients actually get individualized treatment.
Thanks Scott, that was a great blog.