You may have heard that the FDA, after extensive review, decided against approval of a proposed MDMA-assisted therapy to treat Post-Traumatic Stress Disorder.
On the heels of that news, we learned that three research papers from Lykos, a major driver of the movement to medicalize psychedelic drugs, had been retracted for ethics issues. Here’s that story, from an industry website without a paywall:
MDMA Papers Retracted for ‘Unethical Conduct’ on Heels of Lykos’ FDA Rejection
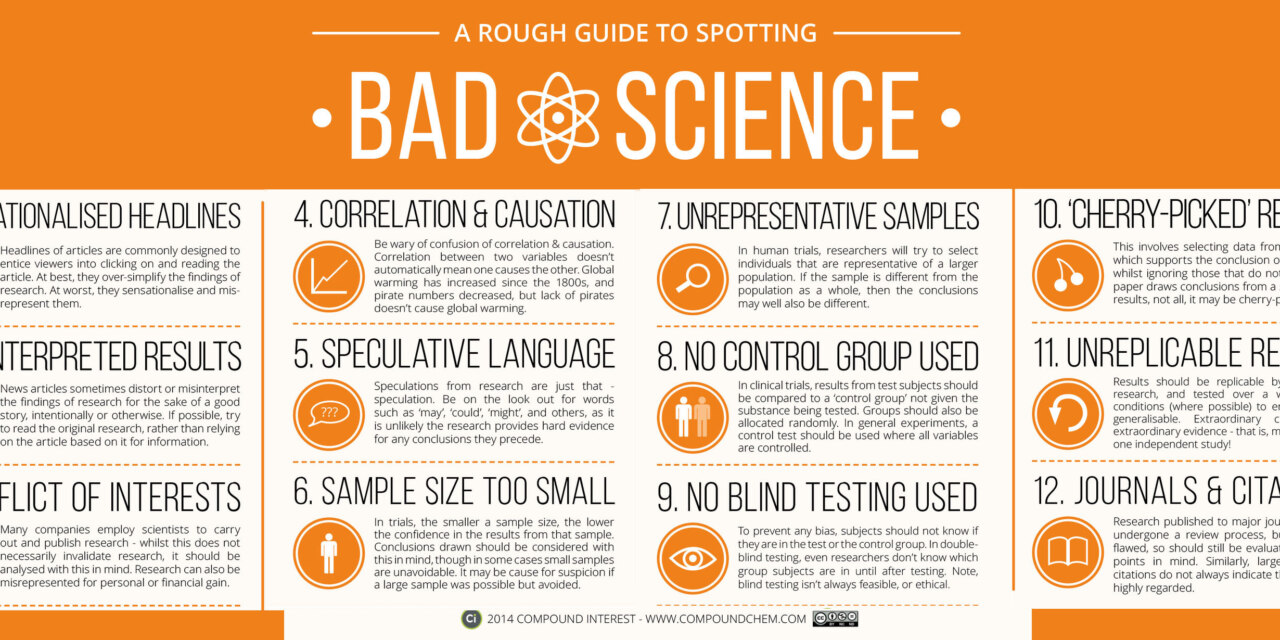
Apparently advocates for psychedelics were genuinely surprised. Maybe they shouldn’t have been, in the wake of an earlier unfavorable report from an independent body, that cited numerous problems with the research evidence — ranging from undisclosed conflicts of interest to questions about the selection of subjects.
Might not sound so awful to lay ears, but in the research world, those can be dealbreakers. In this case, they were.
The consensus: This is only a setback. “No way they give up now,” opined a physician colleague. “Between the V-Cap hustlers and the true believers, they’ll be back. Maybe with psilocybin, instead of MDMA.” By the way, “V-Cap” is venture capital. “Thar’s gold in them thar pills,” he joked.
Advocates sometimes cite the nation’s experience with cannabis legalization as an illustration of how important it can be to legitimize a recognized drug of abuse as a medical treatment. That can pave the way for legal recreational use as well, which is often their real goal.
Not just for personal reasons, either. Recreational use is where the money is.
That may well be the ultimate goal for MDMA and psilocybin, too.
A word about trauma: During my brief association with a trauma treatment program, I realized how diverse the PTSD population really is. There were two broad categories of PTSD patients, which our clinicians treated as separate disorders: One, made up largely of combat veterans and victims of traumatic events such as injuries or violent crime. And a second, composed largely of persons whose stress had been much more prolonged, involved severe abuse or neglect, and usually began in childhood.
The two groups shared certain symptoms, but the trauma they had experienced was substantially different in nature. The therapists felt that simply lumping them together undermined treatment.
If you accept their premise, it makes sense that not all PTSD patients would respond to the same limited range of approaches. That some would benefit from CBT, for example, while others would not.
I imagine that would apply to MDMA-assisted therapy, as well. Some would benefit, others would not.
I guess we’ll need to wait for more (and hopefully, more reliable) outcomes research to finally make up our minds.