There’s a movement afoot to redesign the US methadone treatment system along the lines of that used by other nations, including the UK. It involves significant changes to the rules around who prescribes and dispenses the medication for treatment of Opioid Use Disorders (OUD).
Right now, that’s largely restricted to specialty clinics. With the proposed change, OUD patients would be able to obtain a prescription for methadone from a physician in the office setting, and have it filled by the local pharmacy. The advantages in terms of convenience should be obvious. And from a public health perspective, making methadone easier to get would likely result in fewer unintended overdoses.
I’m old enough to recall the era when it wasn’t unusual for a heroin addict to report several previous overdoses on assessment. None fatal, obviously. One patient dismissed his ODs as ‘no big thing, you just go to sleep for a while, then wake up again.’
Fentanyl has changed all that. Now the emphasis in public health is less on the quality of recovery and more on our desperate need to save lives.
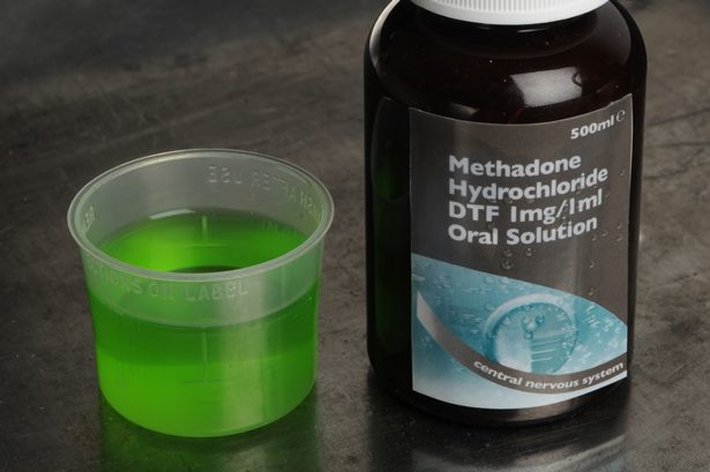
As for the British model, here’s the information the NHS gives potential patients considering methadone for OUD.
Surprisingly– or maybe it’s not so surprising– existing methadone clinics appear to be against the get-your-own-prescription change. Here’s an article on the debate, reprinted from The Washington Post:
As drug deaths soar, experts urge expanded access to methadone
According to the article, the clinics see a loosening of regulations around methadone as encouraging diversion of the drug into illegal use, where it will become yet another part of the opioid problem. They have a point, obviously. Methadone is an opioid, after all, and we’ve seen that happen with medications of the type when they’ve escaped to the streets. Including heroin.
On the other hand, there are plenty of complaints about the current system of specialty methadone programs. For one thing, there aren’t enough of them around to be truly accessible for clients — especially outside large urban areas. The opioid epidemic hasn’t been confined to big cities, and is actually worse in some rural communities. Yet when one clinic closes (usually for financial reasons), rural patients are often forced to travel long distances, sometimes daily, for the drug they’re dependent on.
Because without it, they experience methadone withdrawal — which, according to many patients, is far more severe and debilitating than anything they experienced from heroin itself.
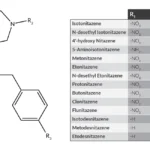
We do have an alternative: buprenorphine. It does much the same things for an OUD patient yet is generally thought to be less sedating and perhaps less harmful when abused. Bupe has already replaced methadone as the medication of choice in many inpatient detox centers, in large part because access is so much easier. The proposed change in the law would put methadone on much the same basis.
One problem: there are now currently some 300,000 Americans on methadone maintenance, and I’m assuming many of those will not want to transition to buprenorphine. They may be on high-dose regimens of methadone and fear withdrawal if and when they attempt to switch.
I don’t favor either side on this particular issue, because I see problems with both models. It’s reassuring that the newer model has been used with some success in Europe. But my experience is that many ideas that do well overseas struggle in the very different cultural and social environment that is America. And in our weird healthcare system, which in many respects, is not really a ‘system’ at all.
I am willing to bet that whatever the resolution turns out to be, some folks, maybe a lot of folks, will be unhappy. As Kurt Vonnegut would say, “so it goes.”