I came across an article on a medical website by a practicing physician who complained about having to complete a brief course as a condition of prescribing opioids to her patients.
Her complaints centered on 1) Having to take the training three times because she practiced in three different states, and 2) Having to pay for the training three times over. Plus it was apparently boring. She describes it in terms of eight hours she’ll never get back.
Besides, she argued, she has no record of problems with opioid prescribing, and doesn’t even use opioids outside of cases where the need is abundantly clear. So why burden her with extra demands?
Doctors, especially those with busy practices, don’t have much time for duties or responsibilities that aren’t clearly necessary to their work. And this physician is convinced that a dull, repetitive training on opioids doesn’t qualify.
Having been through a number of dull, repetitive trainings in my own life, it’s hard not to be sympathetic.
And it’s true, as she points out, that over the past decade, prescription opioids have been replaced by the illicit variety as drugs of abuse, and it’s those that now account for most of the ever-rising overdose statistics.
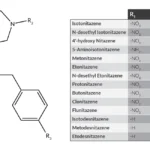
I imagine the DEA devotes most of their time and energy trying to corral illegal sources. Still, “pill mills” do continue to exist, if not in the numbers they once did. I suppose they could stage a comeback — the basic economics still work, unfortunately:
I haven’t forgotten how we came to this point in the opioid epidemic, and the important role that the healthcare professions, including physicians, played in its origins.
You know the story. A transparently self-serving ‘educational’ campaign on behalf of the makers and distributors of prescription opioids was nonetheless successful in erasing awareness of the very real risks associated with opioid use — risks that, after all, had plagued humanity for centuries.
As an addictionologist put it, after one such presentation at a medical conference: “This will not end well.” It hasn’t.
I can relate with the good doctor’s desire to make the education requirements more user-friendly — less repetitive, more affordable, with updated information. That’s just common sense. We know that compliance goes up when training is more directly relevant to the needs of the trained.
And though mandates of every kind are viewed as at least somewhat inconvenient by those who are mandated, they can still be of use in improving care and preventing serious errors — like the catastrophic ones we made around the use of prescription painkillers.
So as the signs say, please excuse the inconvenience as we work to improve our services.