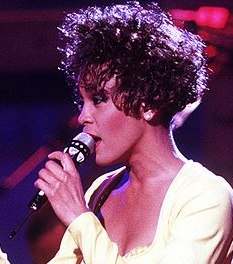
There’ve been a number of stories in the news about Wendy Williams, the once-popular daytime talk show host who has been diagnosed with “primary progressive aphasia and frontotemporal dementia (FTD)”. Contributing factors are said to include a long history of alcoholism. Her neurocognitive deficits are severe enough that any hopes for a return to television are now on hold. Likely for good.
Although heavy drinking was clearly a factor, a precise cause for her difficulties with memory, communication and reasoning is more difficult to establish. Other conditions were present, turning dementia into something of a chicken-or-egg question. Here’s a link to a more detailed analysis:
There’s not much doubt about the impact of chronic alcoholism on brain function, though. A second article quotes a number of people who worked with her on a daily basis: Wendy Williams Struggled with Alcohol During Her Show: ‘She Would Be Drunk on Air,’ Says Source
I suppose none of her staff or colleagues thought of seeking professional help. An intervention, for instance. Or perhaps they considered it but decided it was not their place to interfere. Maybe they were scared of her reaction. People around the drinker often are.
One family I worked with was extremely fearful of the ferocity of the response from their father, a retired colonel known for his sudden rages and deep scorn for any kind of weakness in others. Imagine my surprise when, in the aftermath of a successful intervention, I met up with him for the very first time — in rehab. He turned out to be a smallish, sickly gentleman with barely enough energy to push himself to his feet to shake my hand. I found myself wondering why his two strapping adult sons hadn’t simply picked him up and carried him to the hospital before it was too late. Never mind an intervention.
He was that weak, and that confused.
We seemed to see quite a few patients in those days who suffered from varying degrees of alcoholic dementia. One man had been hospitalized half a dozen times before the true extent of his cognitive problems emerged. Prior to that, the nursing staff regarded him as a bit goofy but still quite functional, perhaps because his verbal abilities seemed intact. The thinking processes behind them, however, were not.
Then came the day when I found him in an armchair in the patient lounge, staring anxiously up at the ceiling. I asked how he was doing and he replied, “Don’t worry, I’ll be all right once we get up in the air.”
He thought he was at the airport, waiting for his flight to be announced.
At one time there was a dedicated residential unit for men with alcohol-related dementia at one of our big State hospitals. Our docs referred their share of older males there, with generally good results. There wasn’t a whole lot of emphasis on treatment, but the care and supervision they received was the antidote for their persistent anxiety. They knew they were safe. That turned out to be most of the battle.
As America grows older, this might be a good model to follow. The cost of such programs isn’t extreme, certainly not when compared to acute hospitalization. And the value to anxious family members? That simply can’t be overstated.