Here’s a very intelligent look at what can happen to a maintenance client when disaster strikes and access to methadone is cut off. It includes the author’s own experience during a historic flood, as well as a discussion of the larger problem, illustrated by the hurricanes in Houston and Florida:
They were opioid addicts on their way to recovery. Then the hurricane hit.
It happens more often than you might think, and mostly never makes the news. One instance I recall: A maintenance client whose current dose was 250 mg, or about twice the clinic’s average, found himself stranded in his apartment by a crushing snowstorm. He managed to procure a bottle of prescription opioids from a neighbor (I don’t know if they were borrowed or bought or he just helped himself), and in the grip of withdrawal, he decided to crushed and inject a large number of pills. But he didn’t feel any substantial effect. At first, he told me, he assumed that must be because the pills were fakes. Then it occurred to him that his methadone-driven opioid tolerance might be so high that he simply couldn’t overcome it.
In hindsight, the experience may have influenced his decision to taper off maintenance.
Another example: A rural methadone clinic was forced to shut its doors because it couldn’t make ends meet– fairly common where reimbursement for maintenance doesn’t meet expenses, and the program can’t attract enough patients to make up the difference through sheer volume (one reason why urban maintenance clinics often have a huge census). There were no local alternatives so the clinic wound up shuttling dozens of clients sixty miles each way for dosing. In the end, many clients had to relocate to other cities.
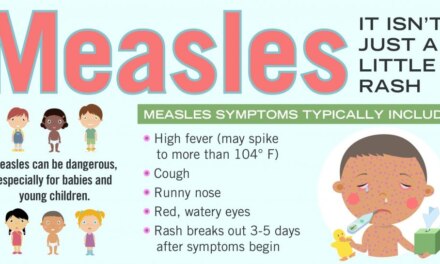
It’s inherent with any maintenance situation, whether we’re talking about insulin for diabetes, dialysis for kidney disease, or psychotropics for serious mental illness. In the case of opioid addiction, the penalty is withdrawal. As the article suggests, the withdrawal experience is augmented by anticipatory anxiety, turning the whole experience into something along the lines of a sustained panic attack. Opioid withdrawal isn’t life-threatening, but just try convincing somebody on methadone when they’re facing a fifth or sixth day without the drug.
And there’s always the risk that a desperate client will OD on fentanyl.
To me, this will always motivate some clients to taper off, since unlike the diabetic or the kidney patient, the outcome isn’t medically contraindicated. That’s why I’d welcome more research into the tapering process, with an eye to improving success rates. I’m not talking about forcing people off maintenance. But when someone has done well and feels ready to taper off, I’d like to think we’re able to help them.