Here’s a helpful piece from The Washington Post on the practical aspects of managing withdrawal from benzodiazepine drugs.
What patients — and doctors — should know about ‘benzo’ withdrawal
It’s one of those health issues that most people, even regular users of benzos, don’t know much about. Why bother? they ask themselves . It’s not like these drugs are addictive.
But of course, they can be. And not infrequently are.
Take the case of actor Burt Reynolds, prescribed Halcion (triazolam) for insomnia. Worked at first, then he found himself increasing the dose, on his own, until he was taking four or five pills at a time — up to sixty a day. That’s a familiar story to anyone who works in addiction treatment, a classic example of loss of control. Accompanied by the need to consume more and more to achieve less and less of the original effect.
Meaning most nights, I suppose Reynolds still couldn’t sleep.
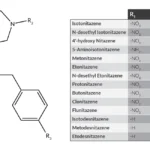
There’s a second, less obvious type of benzodiazepine addiction that is more akin to the maintenance pattern of alcoholic drinking or opioid dependence. The principal problem is a painful, extended withdrawal syndrome. Curiously, medical practitioners had difficulty accepting that some patients could experience significant withdrawal at what seemed to them like lower doses.
I recall a phone conversation with a noted psychiatrist — himself an expert in addictions — who insisted that withdrawal simply wasn’t possible at low doses of benzodiazepine sedatives. We just happened to have such a patient in treatment at that very moment, so I volunteered to arrange a meeting. “I’m sure she’d be happy to share her experience,” I told him.
As far as I know, he didn’t take me up on the offer.
Per the Post article, some 30 million people use benzodiazepines to quell their anxieties or to help them get a good night’s sleep. Research indicates that they’re effective — for a week or two. After that, most of their effectiveness will have eroded. If someone is still taking them on a daily basis, it’s probably an indication of growing dependence. At some point, their motive for taking the drug is simply to relieve the discomfort that appears in its absence.
Depending on how much is used and for how long, benzo withdrawal can be quite serious. And protracted.
That’s why a gradual taper is strongly advised. Often a matter of months, not weeks. As the article notes, a certified addictionologist is likely to be more experienced in managing withdrawal than other physicians. Here’s a partial list if you’re interested:
And for a wise overview of the process, try this link to an informational website: Benzodiazepine Information Coalition